Sunday, October 11th
I am still playing catch with my journal entries and as of this writing it is Tuesday, the 13th of October. It is a wild, wet and windy morning here in The City. The predicted storm generated from remnants of Typhoon Melor hit last nite and it is now a steady rain with gusty winds but a mild 57 degrees. There are over forty thousand people without power and there had been a least one fatality.
Now, back to Sundays' journal.
Ed and I had made arrangements earlier in the week to go hiking. We settled on Samuel P. Taylor State Park in Marin County. It is about a 30-45 minute drive north of The City and the park is not too far from the city of Fairfax.
In order to insure against bonking on the hike I decided to go back to Sunflowers and have some lunch.
Click on the photos below for a larger image.

This is the interior of Sunflowers at Connecticut and 18th. I got there about noon.

A view of the intersection from Sunflowers. On the right corner is Lingba Lounge which I plan to check out before I head home. On the left corner is Aperto restaurant.

I thought this was interesting. A 30 something lady cyclist wearing a mini-skirt, high-heeled boots and day pack and holding a cup of java in her left hand. A very San Fran/Seattle scene.
NOTE: "A few years ago in Denmark we saw lots of women in high heels riding bicycles".
From friend Sandra in Virginia
The bus in the background is the now defunct 53-Southern Heights. This line was recent casualty of the ill conceived plant to save money by reducing service to people who don't/won't can't drive cars. Ridiculous.
Read about all of the Muni Obituaries - 2009

My lunch choice was a simple one. Chicken noodle soup (6.95) with optional mixed veggies (1.00). The rice noodles are hidden below the veggies.


Vietnamese and Thai restaurant soups come with Thai basil, mung bean sprouts and sliced hot peppers as a garnish.
Tasty and filling I felt confident it would fuel me through most, if not all of the hike.
I walked the two blocks back to Bruce's, got my stuff together and then waited by the front door for Ed to arrive.
Ed, my hiking and dinner companion was a college pal of good friend Jerry. Jerry used to teach at WVU in Morgantown. Jerry put Ed and I in touch with each other via email and I am glad he did. Ed has been good company and he had generously offered to pick me up at Bruce's place and drive up to "SamPTay" as we used to call it.

We got to the park and eventually found the trailhead for the Barnabe Lookout Trail which wound up the mountain through mostly Oak and scrub savanna. As we huffed and puffed up the hill we were both glad it had turned out to be a cool, foggy day.
Near the summit we stopped and talked to a group of 5 who had come up the mountain via a different trail. It appeared to be a mom, pop and three grown kids outing, but I can't be sure.

At the summit we stopped for food and water. The fog which was rolling in limiting the view and the wind had picked up a bit. We cooled down quickly it was not long before I had my fleece pullover back on.

This "tree" is actually some sort of communications tower. The photo was taken standing next to a much larger Com facility with a substantial building and a fair sized tower with antenna array.

Our view from the summit.

After refueling we headed back down the hill. It was a quick and easy decent down to Lagunitas Creek and the Redwood Groves there.

This is one of the pedestrian bridges over Luganitas Creek. The creeks have been low, and the Salmon have been stranded in some places. Predicted rains should help alleviate this problem.

I had asked Ed if he would mind stopping at the entrance sign and snapping a picture of me. So, here I am, 40 years later, just a short distance from where my brother Wayne and I nearly met our demise.
The Hemlock Incident
The year was 1969. All 4 of us Breiding Boys - Sutton, myself, Wayne and William were on a field trip with the Shire School, and alternative school which was based in a warehouse somewhere in The City.
The "teacher" Gene had decided it would be educational to take the 4 of us on a trip over to Marin County and explore the woods there. We parked at the gate for the access road for Kent Lake, a reservoir which supplies drinking water to Marin County. The woods was lush and thick with small tributaries feeding into the main stem of the creek from the lake.
At some point we came across a plant we all knew from home. We told Gene it was in the carrot family and it had a sweet tasting, carrot like root which we had eaten before. The plants we had found here at the Park were much, much larger than the plants we had back home. But, we attributed that to the fact they were growing in Californian. Why, I don't know.
We wrestled several of the plants out of the ground and began munching away on the sweet, tasty roots. We all had some, except Gene.
Shortly after that we all piled back into Gene's 1968 Camaro, which I thought was a really cool car, and started the drive back to San Fran. At some point I told Gene I was feeling sick and felt sure I was going to throw up. Gene found a gas stations and I got out of the car and headed to the bathroom. I never made it. I fell to the ground and became convulsively ill. The last thing I remember was literally being thrown into an ambulance.
I am now unsure of the time line, but around two days later I regained consciousness. As my eyes focused and I became somewhat aware of my surroundings, I felt a sharp pain "down there". My hand went to my privates and to my horror I found there was some sort of tube going up inside of me. At that point in my life I had never heard of a catheter.
I looked around and to my left there was a glass room. Inside of it, was my brother Wayne lying in bed. This was a bizarre scene and it frightened me. I was to find out later this was an isolation unit he had been put in because he had contracted a staph infection.
At some point a nurse came by and of course I uttered the usual question: "Where am I?" She told me we were in the hospital. She said the plant we had eaten had poisoned us and we had been made quite sick. Quite sick meant being in a coma for two days and nearly dying.
Apparently when we got to the hospital no one was sure what to do. As I understand it Gene told them about the plant we had eaten which was the suspected culprit for the nasty turn of events. I think at that point Gene went back to the site with a botanist who collected and identified the plant (Poison Hemlock) which was know to be quite toxic.
But, even with this information the required treatment was not known. The toxic alkaloid had to be isolated and identified and then a treatment regimen devised to try to save us. The end result of this were complete transfusion for my brother Wayne and I and being continuously medicated with dilantin and phenobarbital. It was thought the transfusion would clear the toxin from our systems and the drugs would control the violent convulsions we had been experiencing. The big fear was brain damage. So, to this day I have had a handy excuse for every stupid thing I have done.
Eventually my family came to visit along with other folks. It is all kind of foggy. But, it must have been an awful experience for my mom to go through, not knowing whether her two of your sons were going live or die or be permanently comatose.
Brothers Sutton and William had apparently eaten smaller amounts of the plant and were kept over night and released.
Fortunately, for all of us, Gene had eaten none. If he had, there would have been a good chance he would have suffered the same reaction - while driving. And that might have been the end for all of us.
I am not certain my brother Wayne came away completely unscathed from this incident and it may have played a role in why he has ended up the way he has.
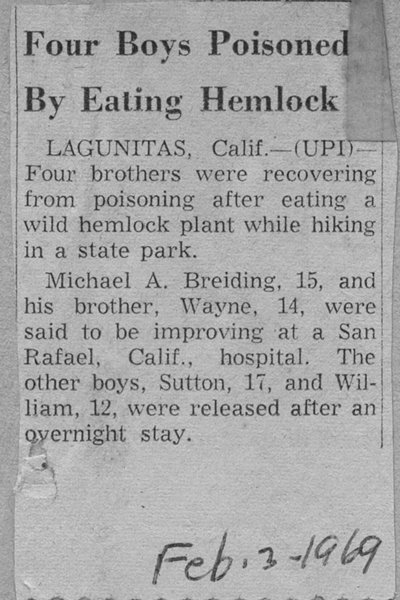
As an aside, this incident was picked up by the wire services and reported in the press nationally.
People who know us personally read about it and some assumed the story ended in tragedy or heard no more about it. So, imagine my surprise, when, the first time I got back to visit Morgantown after a 4 year absence, I find out a number of people thought I was dead.
Fooled 'em...
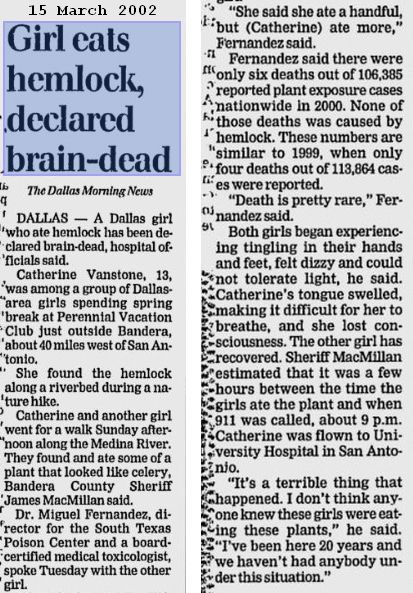
The Breiding Boys were not the only ones to be poisened by water hemlock.
Unfortunately this individual did not fair so well.
NOTE: A web search turned up this report from the journal of California Medicine, August 1973 entitled: "Accidental ingestion of water hemlock. Report of two patients with acute and chronic effects" by D J Costanza and V W Hoversten
Those "two patients" were my brother Wayne and I.
Below is the detailed account of how the poisoning occurred and how it was treated.
California Medicine
The Western Journal of Medicine
119:78-82, Aug 1973Accidental Ingestion of Water Hemlock
Report of Two Patients with Acute and Chronic Effects
David J. Costanza, MD and Vincent W. Hoversten, MD - San FranciscoWATER HEMLOCK
is probably the most poisonous plant that grows in the United States. It is extremely toxic to livestock and to man. In two cases of severe poisoning in humans, the acute phase was manifested by convulsions, uncontrolled neuromuscular movements, respiratory distress, cardiovascular variability, and metabolic acidosis. The long-term chronic effects were electroencephalographic abnormalities and anxiety neurosis.The toxic effects of cicutoxin in man were first recorded by Wepfer in 1679. He reported several children poisoned by the Cicuta hemlock plant and noted "noncoagulation of the blood." In 1814 Stockbridge reported three cases, which were the first in the United States; two of the patients died during violent convulsions. In 1911, Egdahl reviewed the literature and found reports of 47 cases in Europe and the United States.3 The frequency of reports is now much greater and shows that cicutoxin toxicity is still a severe health hazard especially to children. Within the past two years two other reports from divergent areas of the country attest the continued danger of exposure, and poisonings are still reported in Europe.Two cases of accidental ingestion of large amounts of cicutoxin, in which the patients survived but had long-term aftereffects, are reported herein.
In 1969, five boys were hiking in the hills of Marin County, California, when they became hungry and saw a plant that was similar to a known wild edible plant. Two ate several bites of the root (rhizome), which tasted like sweet wild anise, two tasted it and spat it out, and the fifth refused to taste or touch it. Approximately 20 to 30 minutes after ingestion the two boys, who were brothers, became nauseated while driving in the car. They started to salivate, had stomach cramps, and vomited repeatedly. At a nearby gasoline station both boys began to have repeated grand mal seizures. First aid was given and the police delivered the boys to the Emergency Room at Marin General Hospital.
Case 1 (Mike Breiding)
A 15-year-old Caucasian boy was admitted to Marin General Hospital 31 January 1969, 30 to 45 minutes after ingestion of two or three rhizomes of the water hemlock plant, Cicuta virosa. The patient was cyanotic, had widely dilated pupils, and was in obvious respiratory distress. Blood pressure was 130/80 mm of mercury and pulse 120 beats per minute in supraventricular tachycardia. An oral pharyngeal airway was inserted. The patient began to have convulsions and 100 mg of phenobarbital and 100 mg of sodium diphenylhydantoin (DilantinD) were given intravenously, and intravenous infusion of a solution of Ringer's lactate was started. A Foley catheter was inserted into the bladder. The cyanosis disappeared, respiration was labored, and naso-tracheal airway intubation was accomplished. A Bird Mark vu respirator was applied and respiration was continuously monitored. Blood pressure fluctuated between 80/60 and 170/90 mm of mercury and the heart rate varied from 50 to 120 beats per minute. The skin was warm and dry. The muscles were rigid and the pupils dilated widely and then constricted spontaneously. There were also periods of opisthotonos with severe rigid muscle spasms. All of these symptoms were observed repeatedly and seemed to have no relation to each other-they seemed to vary independently. Convulsions continued and pentobarbital sodium, 100 mg, was given every 30 minutes intravenously.After lavage of the stomach, a universal antidote was instilled, and then 8 ounces of potassium permanganate 1:1000 in solution was left in the stomach for 45 minutes and withdrawn. Five percent sodium bicarbonate, 200 ml, was then instilled in the stomach and withdrawn. Convulsions continued intermittently despite treatment with pentobarbital sodium.
About an hour after admission a slight flush developed around the face and neck. Fluctuation of the pupils, clenching of teeth, severe muscle spasms and rigidity, and periodic episodes of severe opisthotonos and intermittent hemiballismic motions continued. Bilateral ankle clonus was present but Babinski and Hoffman reflexes and Wartenberg's sign were absent. The patient was restless and thrashed about. Sodium pentothal, 50 mg, was administered intravenously about 90 minutes after admission; the thrashing diminished in severity, but the convulsive disorder continued. After toxicologic consultation, 3 ml of paraldehyde was administered intravenously over a tenminute period and the convulsions stopped. Blood pressure finally stabilized at 130 to 140/78 to 86 mm of mercury approximately two hours after admission. Maintenance doses of phenobarbital sodium, 60 mg intramuscularly every six hours, were started. Once the convulsions were controlled, the alternating bradycardia and tachycardia subsided, although the cardiovascular events were not directly correlated with the convulsive disorder. The electrocardiogram taken during the convulsive period was within normal limits, showing only sinus arrhythmia.
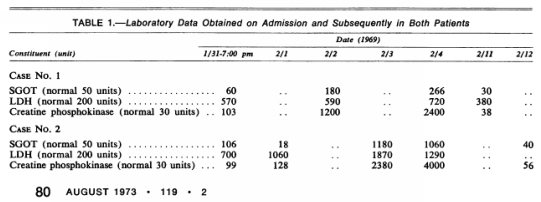
Laboratory data on admission were as follows: serum sodium 137, potassium 3.8, and chloride 99 mEq per liter, carbon dioxide combining power 7 mM per liter, phosphorus 2.2 mg per 100 ml, alkaline phosphatase 1.8 Bodansky units, creatinine 1.1 and blood urea nitrogen 13.0 mg per 100 ml. Bilirubin, amylase, calcium, glucose, albumin, and globulin were within the normal range. Leukocytes numbered 17,800 per cu mm with 62 percent lymphocytes, and the platelet count was normal. The prothrombin time was 15 patient seconds/12.5 control seconds on admission, but follow-up measurements were normal. The serial changes in serum glutamic oxaloacetic transaminase (SGOT), lactic dehydrogenase (LDH) and creatine phosphokinase (CPK) are summarized in Table 1.
Urinalysis revealed transient 2+ proteinuria; 5-hydroxyindoleacetic acid was normal at 3.1 mg in 12 hours.
The patient was rousable after ten hours, but not completely awake until approximately 24 hours after ingestion. He complained of soreness all over his body, particularly in the muscles of the arms and legs. He thought his mind was a little fuzzy but he was not sure about this. An electroencephalogram was very abnormal, showing generalized excess of slowing throughout and a large amount of paroxysmal discharging, more prominent over the frontal areas and exhibiting alternating lateral predominance. A Neurologic Index of Mental Impairment (NIMI) test revealed severe organic mental impairment. There was a steep rise in the levels of creatine phosphokinase and lactic dehydrogenase, which was attributed to muscle trauma secondary to convulsions and rigidity. An x-ray film on January 31 and a second electrocardiogram on February 2 showed no abnormalities. Before the patient was discharged, peeling of the skin on palms and soles was noted. The patient was discharged and Dilantin, 100 mg orally three times a day, and phenobarbital, 15 mg orally four times a day, were prescribed.
Approximately a week after discharge the patient had an acute anxiety reaction and was seen by a psychiatrist. He had hallucinations and visual flashes of white and purple and complained of a feeling of nausea when his eyes were closed. His symptoms were considered partly due to organic flashback and partly due to anxiety neurosis. Approximately three weeks after discharge the patient stopped taking the medications, against medical advice. Results of the two follow-up electroencephalograms and NIMI tests obtained on 11 February and 29 September 1969 were still very abnormal. The last NIMI test showed improvement with a score of 68 percent (normal for 12 years and older, 86 + 7 percent), indicating mild loss of intellectual functioning for his age and grade level. The electroencephalogram on 29 September 1969 was mildly abnormal, showing pronounced improvement with only slight degeneralized and paroxysmal cerebral dysrhythmia.
Case 2 (Wayne Breiding)
A 14-year-old Caucasian boy was admitted to Marin General Hospital 31 January 1969 about 45 minutes after ingestion of part of one rhizome of Cicuta virosa. The patient was convulsing, cyanotic, and comatose. Blood pressure was 138/60 mm of mercury, pulse 84 beats per minute, and respirations wheezing in character between convulsions. Bowel sounds were audible without a stethoscope. The facial skin was flushed. An endotracheal tube was inserted immediately and an intravenous infusion of Ringer's lactate solution was started.The stomach was washed with 8 ounces of potassium permanganate solution 1:1000, and then a 5 percent sodium bicarbonate solution was instilled into the stomach and withdrawn. Simultaneously with the lavage, amobarbital sodium, 0.5 grams, was administered intravenously. Because of persistent convulsions, penthothal sodium, 50 mg, was given intravenously three times about 15 to 30 minutes apart. About an hour and a half after admission the blood pressure was 70/60 mm of mercury but increased spontaneously without vasopressors to 100/70 mm. Because of another convulsion, phenobarbital sodium, 120 mg, was administered intramuscularly. The wheezing and hyperactive bowel sounds ceased and the pupils became normal in size.
The convulsions stopped completely about three and a half hours after admission, but the patient became very active, clenching his teeth, swinging his arms randomly, arching his back, and moving his whole body continuously. He was not responsive to commands. Intramuscular administration of paraldehyde, 3 ml, and another dose of phenobarbital sodium, 120 mg, did not appear to affect the hyperactivity. Therefore, diazepam (Valium@) was administered both intravenously (5 mg) and intramuscularly (5 mg). (By differing the regimen from that followed in Case 1, it was hoped to determine the best means of controlling the recurrent convulsions.) Repeated doses of Valium appeared to control the excessive activity in about 30 minutes. Eight hours after admission the patient continued to have intermittent prominent flushing of the face and body, but a 12-hour urine test revealed a normal level of 5-hydroxyindoleacetic acid. Laboratory data on admission were as follows: serum sodium 144, potassium 4.1 and chloride 104 mEq per liter, carbon dioxide combining power 7 mM per liter, phosphorus 2.7 mg per 100 ml, alkaline phosphatase 3.0 Bodansky units, creatinine 1.5 and blood urea nitrogen 13 mg per 100 ml, and amylase 375 Somogyi units per 100 ml. Glucose, calcium, bilirubin, albumin, and globulin were all within normal limits. Leukocytes numbered 21,000 per cu mm with 58 percent lymphocytes, and the platelet count was within normal limits. The leukocyte count returned to normal by the fifth day. Serial changes in SGOT, LDH, and CPK are summarized in Table 1.
About 30 hours after admission the patient wakened enough to ask what had happened. His muscles were very sore and the skin on his face was scaling almost as if he had been sunburned. Both conditions lasted for several days. On the second hospital day his temperature rose from normal levels to 39.4°C (103°F) and rhonchi were heard in his chest. The chest roentgenogram was clear but Hemophilus parainfluenza was cultured from the throat. Tetracycline therapy, 500 mg four times a day, was carried out until all evidence of infection disappeared. On 4 February 1969 an electroencephalogram showed prominent variable slowing throughout, with irritative features, and a NIMI test revealed decided intellectual impairment. Although still weak, the patient was discharged February 13. At this time both the creatine phosphokinase and serum glutamic oxaloacetic transaminase levels were still a little above the normal range.
With the exception of occasional nightmares, no specific psychiatric problems occurred after discharge but an electroencephalogram taken 27 February 1969 was still abnormal although the NIMI test taken at the same time was within normal limits.
Discussion
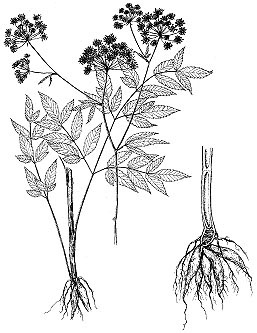
Water hemlock, cow bane, five-finger root, "snake weed," "wild carrot," or Cicuta virosa (Cicuta maculata, Cicuta vagans) is of the botanical family Umbelliferae. It is a perennial plant with large compound leaves and clusters of fleshy roots (Figure 1) and is related to the parsley family. The plants are usually found in marshy ground around ponds or ditches. They may be mistaken for wild parsnips, artichokes, celery, sweet potatoes, and, in our case, sweet anise.Cicutoxin (an unsaturated aliphatic alcohol) is the toxic component of Cicuta virosa and is found in all parts of the plant, but the greatest concentration is in the root stock or rhizome. The usual lethal dose in an adult is one rhizome, although whistles made from the hollow stems of the plant have caused deaths in children. A piece of root the size of a walnut has been known to kill a cow, and a single root has been known to kill a horse.
Usually nausea, salivation, emesis, and tremors develop within 30 to 60 minutes after ingestion. Abdominal cramps and projectile and violent vomiting occur, and severe convulsions ensue. Death results from exhaustion and respiratory paralysis. Retrograde amnesia has been reported to be not uncommon upon recovery, but so far as could be determined serial electroencephalograms and tests of mental function have not been reported heretofore.
Clinically we observed previously reported toxic reactions: salivation, nausea, projectile vomiting, abdominal cramps, restlessness, rigidity, opisthotonus, convulsions of severe and violent nature, widely dilated pupils, trismus, and retrograde amnesia. Additional physiologic effects that have not been reported elsewhere were hemiballismic type motion, localized flushing, and subsequent peeling of facial skin and of palms and soles. The pronounced and varied reactions of the cardiovascular system observed in the two cases herein reported, including bradycardia, tachycardia, hypotension and hypertension, agree with clinical observations of Egdahl and Statton and the pharmacologic studies of this toxin by Grundy and Howarth. In addition, Withers et al reported no detectable pulse and demonstrated hypotensive effects in dogs when 95 percent ethyl alcohol extract of hemlock root was administered intravenously.
Of the abnormal laboratory data, the very low bicarbonate level probably resulted from metabolic acidosis and was possibly accentuated by respiratory alkalosis, although plasma pH was not determined. The high creatine phosphokinase levels reflected the severe muscle rigors, rigidity, and convulsions22 and the lactic dehydrogenase levels also revealed a moderate elevation of LDH isoenzyme fraction 5, suggesting liver or skeletal muscle damage. We believe that the persistence of these levels was attributable to severe muscle involvement in the convulsions, although we cannot be certain that direct muscle toxicity was not present. Elevated enzyme levels after convulsions are well known and they have been observed after convulsive shock therapy. The increased prothrombin time in Case No. 1 is unexplained but may be due to liver involvement. Proteinuria was transient and may have been a nonspecific reaction of the toxin.
We found that Valium was more effective than paraldehyde or barbiturates in controlling the severe uncoordinated muscular movements of the acute phase. We were not able to evaluate or compare these drugs adequately with regard to their effectiveness in controlling seizures, but both were effective. It was a relief to know that we had drugs to control these seizures and movements which were the wildest and longest convulsions in the experience of those on the medical and nursing staff attending these patients.
We conclude on the basis of the abnormal follow-up electroencephalograms and NIMI tests and the psychiatric evaluation that the toxic effects on the psyche and cerebrum were not transient. Chronic cerebral and psychiatric effects have not been reportect heretofore. During the early convalescent period, one patient (Case 1) had dreams, fears, a feeling of non-wellbeing, attacks of acute anxiety, and visual phenomena. The electroencephalograms, NIMI tests, and clinical observations indicated severe organic mental impairment that persisted for several months.
ACKNOWLEDGMENTS
The Fairfax Police Department responded promptly to the emergency and gave excellent first aid. Professor Lincoln Constance of the Department of Botany, University of California, Berkeley, California identified the plant and rhizome, after the California Highway Patrol had swiftly taken them to him.
- REFERENCES
1. Wepfer JJ: Cicutae Aquaticae historia et noxae. SM 40 Basileoe, J. R. Konig, 1679- 2. Stockbridge J: Account of the effects of eating a poisonous plant called Cicuta maculata. Boston Med Surg J 3:334-337, 1814
- 3. Egdahl A: A case of poisoning due to eating poison hemlock (Cicuta maculata). Arch Intern Med 7:348-356, 1911
- 4. Rork LE: Plant poisoning in a child. Rocky Mountain Med J 66:4749, 1969
- 5. Withers LM, Cole FR Nelson RB: Water hemlock poisoning (Letter to the Editor). N lngl J Med 281:566-567, 1969
- 6. Robson PMB: Water hemlock poisoning. Lancet 2:1274-1275, 1965
- 7. Vitale JH, Steinhelber JC, Drake WG, et al: Psychological dimensions of cerebrovascular insufficiency. Percept Motor Skills 29:555-563, 1969
- 8. Statton MR: Water hemlock poisoning. Colorado Med 16: 104-111, 1919
- 9. Sampson AW, Malmsten HE: Stock poisoning plants of California. Univ Calif College of Agriculture, Agriculture Experiment Station Bull No 593, Rev 1942, pp 3-90
- 10. U.S. Department of Agriculture: Twenty-two plants poisonous to livestock in the Western states. Agriculture ILnfo Bull No 327, 1968
- 11. Huffman WT, Moran EA, Binns W: Poisonous plants. U.S. Department of Agriculture, Yearbook of Agriculture, 1956, pp 118-130
- 12. Von Oettingen WF: Poisoning: A Guide to Clinical Diagnosis and Treatment, 2nd Ed. Philadelphia, W. B. Saunders, 1958, p 304
- 13. Arena JM: Poisonous plants. Emergency Medicine, May 1970, pp 1741
- 14. Gompertz LM: Poisoning with water hemlock (Cicuta maculata)-Report of seventeen cases. JAMA 87:1277-1278, 1926
- 15. Kingsbury JM: Poisonous Plants of the United States and Canada, 3rd Ed. New York: Prentice Hall, 1964, p 377
- 16. O'Leary SB: Poisoning in man from eating poisonous plants. Arch Environ Health 9:216-242, 1964
- 17. Lampe KF, Fagerstrom R: Plant Toxicity and Dermatitis, Vol 2. Baltimore, Williams and Wilkins, 1968, pp 129-132
- 18. Miller MM: Water hemlock poisoning. JAMA 101:852-853, 1933
- 19. Hagerty DR, Conway JA: Report of poisoning by Cicuta maculata, water hemlock. New York J Med 36:1511-1514, 1936
- 20. French SP: Poisoning by hemlock. Boston Med Surg J 74: 428429, 1866
- 21. Grundy HF, Howarth F: Pharmacological studies on hemlock water dropwort. Br J Pharmacol Chemotherap 11:225-230, 1956
- 22. Savignano T, Hanok A, Duo J: Creatine phosphokinase activity-A study of normal and abnormal levels. Am J Clin Path 51:76-85, 1969
- 23. Goodfriend TL, Kaplan NO: Isoenzymes in clinical diagnosis. Circulation 32:1010-1019, 1965
- 24. Batsakis JG: Serum enzymes and diseases of the cardiovascular system. In: Laboratory Scope, Vol I, Kalamazoo, Mich., The Upjohn Co, Jul 1969, ppt 2-17
- 25. Hunt D, Bailie MY: Enzyme changes following direct current counter shock. Am Heart J 76:340-344, 1968
- 26. Robinson TW: Important advances in clinical medicin Valium in the treatment of epilepsy. Calif Med 112:63-64, Mar 1970
- 27. Parsonage MJ, Norris JW: Use of diazepam in the treatment of severe convulsive status epilepticus. Br Med J 3:85-88, 1967
- 28. Bowe J: Status epilepticus and diazepam (Letter to the Editor). Br Med J 1:439-440, 1969
- 29. Howard FW Jr, Seybod M, Reiher J: The treatment of recurrent convulsions with intravenous injection of diazepam. Med Clin N Am 52:977-987, 1968
- 30. Bennett JV: Tetanus-The role of diazepam in therapy (Editorial). Calif Med 115:51-52, Oct 1971 82
PDF: California Medicine: The Western Journal of Medicine 119:78-82, Aug 1973
ADDENDUM:
"You may have forgotten, but the story I heard at the time was that you had overdosed on LSD and was a living vegetable." -CP
My thanks to Ed for helping me conjure up all this by making the trip to SamPTay possible and thus giving me a reason to finally put it all down on "paper".